What Is the World Health Organization?
What is the WHO? Learn how the UN agency in charge of international public health responds to crises that threaten global health coordination, such as the COVID-19 pandemic.
In late 1918, saloons, dance halls, and cinemas shuttered across the United States. Streets were largely empty. Many cities required residents venturing outdoors to wear masks. The millions who remained indoors grew lonely as months of quarantining wore on.
Does that sound familiar?
Then, as during COVID-19, the world was battling a deadly pandemic. The disease, commonly known as the Spanish flu, claimed roughly fifty million lives in just six months. The pandemic inflicted a greater death toll than World War I.
Though the world found itself in a similar situation with the COVID-19 pandemic, the tools used to fight global health challenges have evolved. Specifically, the formation and expansion of the World Health Organization (WHO) has changed the way the world handles the threats of infectious diseases.
This resource examines the WHO’s mandate and explores the obstacles that threaten global health coordination.
What is the WHO?
Global health challenges recognize no borders. As a result, fighting the spread of diseases requires not only strong domestic policies but also international cooperation. Such cooperation began in earnest following World War II with the creation of the WHO. As the preeminent authority on global health, the WHO is responsible for coordinating responses to various threats, including border-hopping diseases. However, the COVID-19 crisis has highlighted the agency’s shortcomings. Most notably, the organization has been unable to hold members accountable and suffered from serious funding challenges.
A short history of the WHO
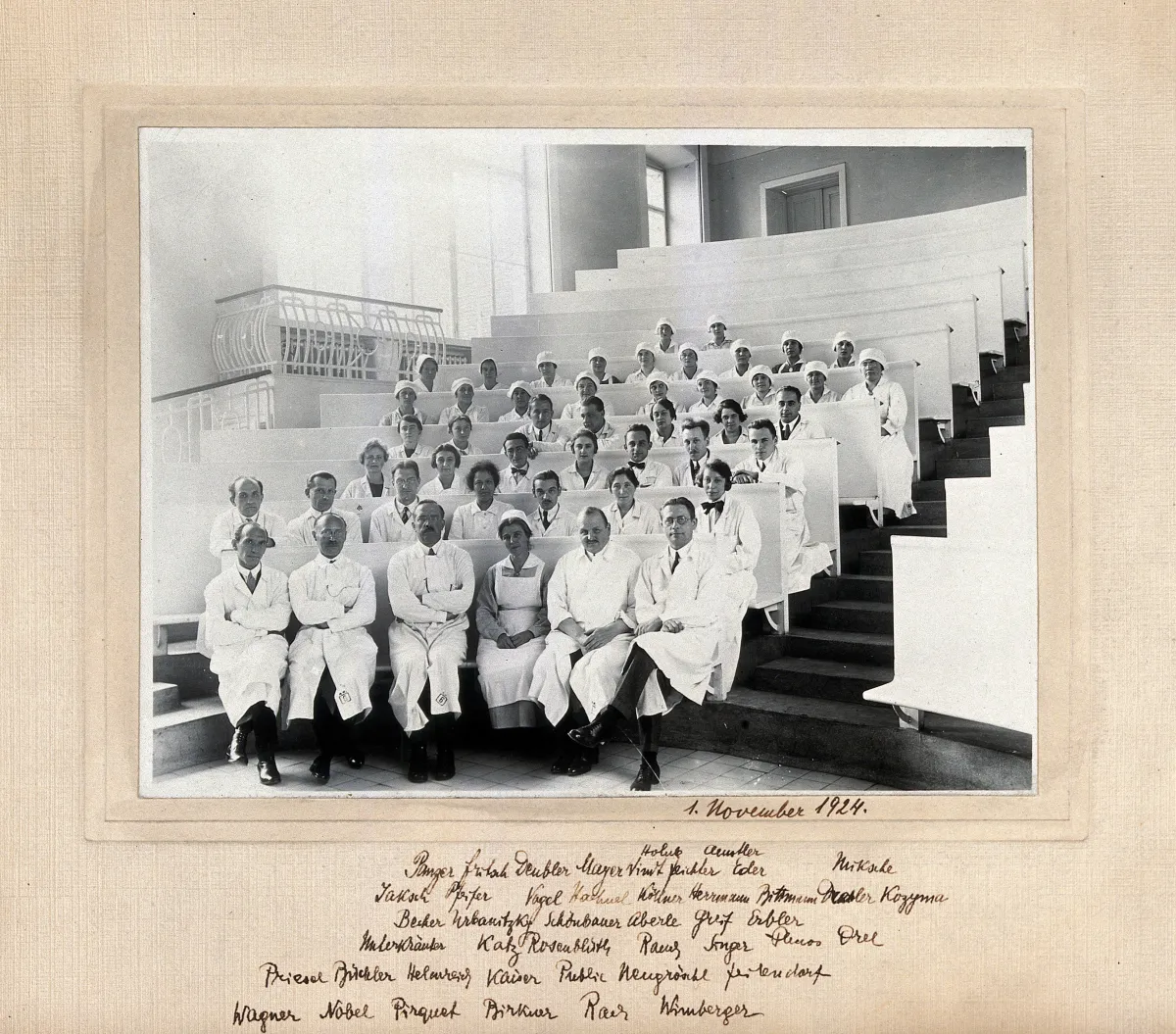
Although the World Health Organization typically takes a leading role in coordinating international efforts to stop the spread of diseases, the organization has several predecessors. As far back as 1851, doctors and diplomats from twelve European countries gathered in Paris for the first International Sanitary Conference. This event marked a milestone for countries cooperating on cross-border health issues. Several predecessors to the WHO followed, including the Pan American Health Organization (PAHO) in 1902, The Office of International Public Health (OIHP) in 1907, and the Health Organization of the League of Nations (HOLN) in 1919. When countries joined together after World War II to form the United Nations, they created a single global health authority: the World Health Organization, which absorbed the HOLN, OIHP, and PAHO.
What does the WHO do?
Founded in 1948, the WHO is a UN agency. Its mission is to pursue “the attainment by all peoples of the highest possible level of health.” Today, the WHO mission translates into work such as malaria prevention, combating obesity, and monitoring the health consequences of issues like climate change and genetically modified foods. Although contagious diseases like COVID-19 attract the world’s attention, much of the WHO’s work focuses on diseases such as cancer or diabetes that aren’t transmitted between people. Those are called noncommunicable diseases, and they account for 74 percent of the world’s deaths.
The WHO partners with national health agencies and nongovernmental organizations (NGOs) to tackle local health challenges. It doesn’t provide direct medical care; rather, it equips health agencies with resources, such as medicine and protective equipment. The WHO also provides guidance on how to effectively deliver health care. Those local projects are wide ranging and include advising on tobacco taxes in Angola, electronically surveilling public health in Jordan, and reporting road traffic fatalities in Thailand.
International Health Coordination in Action: Polio, HIV/AIDs, and COVID-19
In addition to assisting with country-specific challenges, the agency coordinates global responses to international health crises such as epidemics and humanitarian disasters. The WHO has helped nearly eradicate polio and has provided millions of vaccine doses in response to outbreaks of cholera, meningitis, and yellow fever. One of the agency’s biggest successes was coordinating mass smallpox vaccination campaigns, which culminated in the eradication of the disease in 1980. The WHO’s campaign is credited with saving hundreds of millions of lives.
However, the WHO has not always succeeded. In the early stages of the HIV/AIDS epidemic, WHO staff downplayed the severity of the crisis. After years of WHO inaction, world leaders created a new agency—the Joint UN Program on HIV and AIDS (UNAIDS)—to spearhead the global HIV/AIDS response. The formation of a workaround organization demonstrated that the WHO does not have a monopoly on global health interventions. While the WHO was a cosponsor of UNAIDS, it did not lead the initiative.
The WHO has also struggled to address one of the biggest public health challenges of this century: COVID-19. The agency’s pandemic response involved delivering medical equipment, organizing global data, issuing broad public health guidelines, and creating response plans in partnership with national health agencies. But even though the WHO issued guidelines—like recommendations on mask-wearing—they didn't have the authority to force countries to comply.
Can the WHO enforce guidelines on members?
Why do countries choose not to follow WHO guidelines that are designed to save lives? Often, they feel those guidelines run counter to their national interests. For example, some countries prioritize their own citizens by stockpiling medical supplies rather than following WHO guidance and trading with countries in the greatest need.
The WHO has few tools to enforce its guidelines as it relies on countries’ voluntary participation. That inadequate enforcement structure became evident early in the COVID-19 pandemic. In defiance of the WHO’s recommendations, certain countries placed trade restrictions on medical supplies to ensure care for their own citizens.
Additionally, the WHO is responsible for coordinating the detection, assessment, and reporting of public health emergencies following the International Health Regulations, a legally binding agreement signed by all WHO members. However, the agency’s limited enforcement powers leave it unable to mandate regular and robust disease surveillance from member countries and rely on governments to self-report infection numbers. Those reports can be delayed or inaccurate—either intentionally, if a country wants to downplay an outbreak within its borders, or simply because of faulty disease-reporting systems. The WHO faced extensive criticism for relying on that flawed system during the 2014 Ebola crisis in West Africa and the COVID-19 outbreak in China. Slow, inaccurate, or intentionally misleading disease reporting from member countries delayed the global response to each health crisis.
How is the WHO’s funding constrained?
Limited enforcement power is not the WHO’s only obstacle. Funding and financial constraints pose a challenge as well. The agency has an extremely broad mandate to fulfill, but it often lacks the budget and staff.
WHO member countries pay annual dues, which account for approximately 20 percent of the organization’s budget. The remaining 80 percent comes from the voluntary contributions of countries and private funders like the Bill & Melinda Gates Foundation.
Although voluntary contributions are vital for the functioning of the WHO, they can also come with strings attached. Rather than allow the WHO to set its priorities, many funders require their donations go toward specific projects—a process known as earmarking. Objectors to this practice have argued that such funding weakens the WHO's authority, allowing outside forces to dictate global health priorities. In 2019, for instance, just before the COVID-19 pandemic, only eight percent of the WHO's budget went to activities related to pandemic preparedness. Meanwhile, three times that amount went to eradicating polio, a top priority for the Bill & Melinda Gates Foundation, one of the WHO's largest contributors.
Additionally, critics say the WHO is slow to criticize major donors for fear of jeopardizing its funding. The organization’s director-general, Tedros Adhanom Ghebreyesus, came under fire for praising China’s “transparency” in handling the initial COVID-19 outbreak despite evidence of Chinese officials delaying disease reporting, undercounting cases, and silencing whistleblowers. Journalists, diplomats, and world leaders have said that China’s actions amounted to a deliberate political cover-up to protect the country’s stable and authoritative image.
With much of the WHO’s funding coming from voluntary contributions, one country’s changing politics can throw the entire agency’s operations into turmoil. The drawbacks of that fickle behavior became clear after the United States, the WHO's largest contributor, announced in May 2020 that it would terminate its relationship with the WHO due to the organization’s perceived leniency toward China and mishandling of the COVID-19 pandemic. Without U.S. funding, the WHO stood to lose 23 percent of its budget for emergency health operations in the middle of a global pandemic. The United States reversed its retreat from the WHO in January 2021 under President Biden. However, the incident revealed how vulnerable the WHO is to one country's political upheaval.
What is the future of the WHO?
The world lacked the tools to respond to a deadly pandemic in 1918, but today the global health landscape looks markedly different. The emergence of various foundations, NGOs, national health agencies, and the WHO has changed the landscape for how the world grapples with health crises.
Yet those pieces will not always work together in harmony. Who oversees the response to a public health emergency is not always clear. This is especially true given the world’s top agency faces serious funding and enforcement challenges. The WHO’s inability to organize a fully coordinated response to the COVID-19 crisis led experts to wonder whether the agency requires reform. Some experts even assert that a new international health organization is needed altogether.
What is clear, however, is that coordination and cooperation are more necessary than ever before as the world heads into a future marked by global challenges. Problems related to climate change, mass migration, conflict, and other areas can all interact with and exacerbate public health threats, making global health security an important concern for today’s international order.